Uterine Fibroid Embolization (UFE) as alterntive to hyterectomy FAQs
How Does UFE shrink Fibroids without Surgery? Can UFE be an effective alternative to Hysterectomy?
FAQs about Uterine Fibroid Embolization (UFE)
-
Video By Channel 7 News Team: UFE performed by Dr Eisen Liang-Sydney fibroid embolisation specialist
Watch this video produced by Channel 7 News Team showcasing UFE by Sydney fibroid treaetment specialist Dr Eisen Liang from Sydney Fibroid Clinic
UFE stands for Uterine Fibroid Embolisation, also known as UAE (Uterine Artery Embolisation).
During UFE, small particles are injected into the arteries tof the uterus, blocking the blood flow to the fibroids which will shrink and die.
-
How is UFE performed by Sydney Fibroid Clinic?
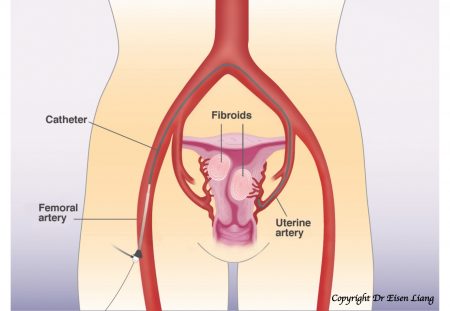
UFE at Sydney Fibroid Clinic is performed by interventional radiologist Dr Eisen Liang who specialises in uterine embolisation. The procedure is not painful and therefor ecan be perfomed under light sedation. Local anaesthetic is injected at the groin, where a tiny nick in the skin is made. A catheter (small tube 1 – 2 mm in diameter) is then inserted into the femoral artery. X-ray dye is then injected to generate a map to guide the catheter to reach the uterine arteries. Tiny plastic particles (0.3 – 0. 5mm in size) are mixed with X-ray dye and injected under X-ray control to block the uterine arteries.
-
How does UFE work? UFE shrinking fibroids without harming the normal uterus?
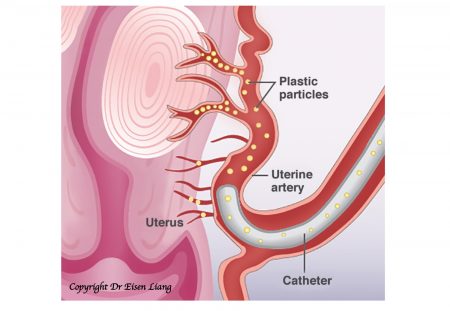
UFE treats fibroids by blocking their blood supply. At Sydney Fibroid Clinic, we inject the well trusted tiny PVA particles into the uterine arteries to sut down blood flow to the fibroids, causing them to shrink and die.
As you can see in the above picture, the normal uterine muscle (myometrium) remains viable and healthy. This is because the normal part of the uterus has a rich network of dormant collateral vessels that can be recruited when needed—such as during pregnancy when the uterus enlarges and requires increased blood flow. These collateral vessels naturally shut down again after childbirth.
When UFE blocks some of the arteries in the noraml part of the uterus, these dormant vessels are recruited and activated to preserve the blood supply to the normal uterine tissue. In contrast, fibroids do not have dormant collateral vessels to recruit, and therefore will die without blood supply.
-
How effective is UFE compare with hysterectomy?
Cochrane review in 2014 cited 5 clinical trials comparing UFE with hysterectomy, concluding that UFE is as effective as hysterectomy in alleviating fibroid symptoms and improving quality of life.
UFE is effective for multiple and large fibroids. All fibroids in the uterus are treated in one go. Unlike myometomy, small fibroids left behind can grow and cause recurrent symptoms. UFE is an one-off treatment and fibroid recurrence afte UFE is exceedingly rare.
Sydney Fibroid Clinic’s own study showed 93% of women treated were happy or very happy with the outcome. The size and number of fibroids do not usually matter to the success of UFE.
-
Hysterectomy vs UFE Comparison Table
Hysterectomy UFE Nature Major surgery Minimally invasive Where Operating theatre Angiogram suite Performed by Gynaecologist Interventional radiologist Anaesthetic General Local Size of cut on skin 15cm 0.3 cm Hospital stay 4 – 6 nights 1 – 2 nights Recovery 4 – 6 weeks 1 week Risk of blood transfusion 2 – 3% Nil Acute complication 5 – 10% < 1% Prolapse Incontinence Risk Yes No Effectiveness for fibroid symptoms Same Same Quality of life improvement Same Same Imaging follow-up No at 6 month Future fertility No Possible Cost Higher Lower -
What are the advantages of UFE over hysterectomy?
UFE is highly effective in treating the symptoms of fibroids without surgical removal of the fibroids or uterus. The procedure is performed under local anaesthetic and is much less invasive than a hysterectomy. When compared to a hysterectomy, UFE requires a shorter hospital stay (1 – 2 days versus 2 – 7 days) and much shorter convalescence (1 week versus 4 – 6 weeks) before returning to work or normal activities. Women can get rid of fibroid symptoms by shrinking their fibroids, instead of having their fibroids or uterus removed by surgery.
UFE can effectively shrink fibroids without the risk of hysterectomy and without the long term side effects of hysterectomy, such as prolapse, incontinence, early menopause, sexual dysfunction, and increased coronary artery disease risk.
-
What are the risks of UFE compare with hysterectomy?
UFE is a minimally invasive procedure. It is very safe, especially when compared with hysterectomy which is a major surgery requiring general anasethetic.
Procedural-related complications are very rare for UFE. Groin haematoma is less than 1%. Other blood vessel injuries are even less common. Non-target injection of particles to other organs should not occur in experienced hands. Bladder infection from catheterisation is around 3%. Major complications that reuiring ICU admission or vascular surgical inervetion are almost unheard of.
Delayed complications are usually related to fibroids located near the uterine cavity (submucosal). Small fibroid fragments can slough off – seen as virginal discharge or passage of small tissue fragments. Sloughing of large tissue fragments into the cavity may cause obstruction of the cervix, resulting in pain and infection (smelly discharge, fever and chills) in about 3% of women treated. Some women are able to pass the fibroid fragments themselves; others might require a transcervical removal (like a curette procedure).
The risk of needing a hysterectomy to treat an uncontrollable infection is less than 1%.
Hysterecotmy is a major operation that is associated with complciations of general anaesthtic and major surgery, including infection, blood loss, and wound issues. Major injuries to the bladder, utreter and bowel are rare but devastating to the patients.
There are also risks of developing long term side effects of hysterectomy including prolapse, incontinence, sexual dysfunction, early menopasue and heart dissease.
UFE are not associated with the acute surgical risks and long tern side effects of hysterecomy. UFE is a much less invasive and safer fibroid treatment option compare with hysterectomy.
-
Is UFE still new and experimental?
No. UFE has been performed since 1995 and has been rebatable by Medicare since November 2006. International and local studies have demonstrated UFE is safe and effective in treating fibroid symptoms. It is recognised as a compelling treatment option by colleges of obstetrics and gynaecology in Australia, the UK and USA. In 2014, Cochrane Review – the highest evidence authority in medicine – concluded that UFE is as effective as a hysterectomy in symptom relief and quality of life improvement.
Dr Eisen Liang of Sydney Fibroid Clinic performed his first UFE in 1997 in Hong Kong and has been performing UFE in Sydney since 2007 when Medicare rebate become available. Dr Eisen Liang of Sydney Fibroid Clinic performs 250 UFE/UAE procedures annually.
-
Is UFE painful?
The UFE procedure itself is essentially pain-free. Local anaesthetic at the groin may sting for about 15 seconds before taking effect. Soon after embolisation, the fibroids are strangulated (cut off from blood supply) and pain may be experienced – but the degree varies from person to person.
Our robust pain control protocol has worked well for many previous patients for more than 10 years, including patient-controlled analgesia (PCA) administered through an IV drip. Pain is usually worst for the first 12 hours and pain is usually controllable with oral pain medication the following day.
Take home medications typically include regular Panadol and nonsteroidal anti-inflammatory drugs (NSAIDs). Additional stronger pain medications are also supplied. Pain should subside within 4 – 5 days and patients should anticipate returning to normal activities about 7 days after the procedure.
-
Will I still get my period after UFE? Will I enter early menopasue?
Women considering UFE/ UAE are concerned about whether the treatment might affect ovarian function or bring on early menopause. The good news is that ovarian injury from UFE/UAE is uncommon, especially in younger women.
How common is ovarian dysfunction after UAE?
Women under 40–45 years old
- Studies consistently show minimal long-term impact on ovarian function.
- AMH levels may dip slightly at 3 months but usually recover by 6–12 months.
(Tropeano et al., Human Reproduction 2011) - Most women continue regular periods and maintain their fertility potential.
(McLucas et al., Fertility & Sterility 2015)
Women 45 years and older
- Women nearing menopause naturally have lower ovarian reserve, so UAE may bring on menopause a little earlier.
- Randomised trials show a 10–20% chance of earlier menopause in this age group.
(Hehenkamp et al., Human Reproduction 2007; de Bruijn et al., AJOG 2016)
Overall risk of permanent amenorrhoea
- Across all ages: 1–7%.
- Under 40: 0–2%.
(EMMY Trial, de Bruijn et al., AJOG 2016)
-
Can I still get pregnant after UFE?
Many prior studies have shown pregnancy is possible after UFE. Overall, meta-analysis suggests that the live birth rate post-UFE is in the range of 31-48%. There is a small risk of ovarian failure of 1-3% following UFE in women younger than 40 years of age. In other words, 97-99% of the time her ovaries are not injured with UFE.
Though a successful pregnancy outcome is possible after UFE, this is a complex issue. The presence of fibroids may make it difficult to get pregnant, cause potential miscarriage and present difficulties with normal vaginal delivery.
Traditionally, a myomectomy is recommended if fibroids are thought to be interfering with fertility and pregnancy. A myomectomy is a major surgery and is generally more technically challenging than a hysterectomy. Risk of blood transfusion is higher than with a hysterectomy and the risk of needing a hysterectomy remains if the surgeon is unable to control bleeding.
For those fibroids unsuitable for a myomectomy or hysteroscopic resection, UFE should be considered as an alterntive or adjnunt treatment.
Following UFE, there is more than a 90% chance that the uterus can be conserved.
However, women younger than 40 needs to be aware about the 1 – 3% risk of ovarian failure. Egg harvesting prior to UFE may be considered as an option. Beware that ovarian stimulation can cause further fibroid enlargement.
It should be emphasised that the aim of UFE is to provide fibroids treatment with a minimally invasive technique, in order to avoid hysterectomy. Although pregnancy is still possible after UFE, successful pregnancy depends on many other factors and therefore cannot be guaranteed.
-
What are the plastic particles (PVA)?
In Sydnehy Fibroid Clinic, Dr Eisen Liang uses PVA (Polyvinyl alcohol) as the blocking agent. It is a pure form of plastic without harmful additives. PVA as embolic material in medicine has been around for more than 30 years. It is chemically inert, and does not react to the bodies chemical or biochemical process. It does not cause allergy.
Clearly there has been plenty of research on PVA.
We’ve seen PVA used in numerous medical settings such as soft contact lens material, artificial heart linings, artificial cartilages, catheters, skin, and pancreas membranes(1). PVA is commonly used as capsules for medicine, vitamins and dietary supplements.
Pharmacologists have explored using PVA as drug delivery systems to distribute medications through various routes effectively. They’ve also harnessed the film-forming and adhesion properties in body washes, multipurpose creams, and sunscreens (1,2).
Researchers and manufacturers continue to explore the potential uses of PVA to keep foods safe. We see PVA in food packaging and commonly used as capsules for dietary supplements. It’s safe to consume in normal quantities, and the FDA recognizes it as a GRAS ingredient(1).
Check out this link for the reference .
-
Is UFE effective for adenomyosis?
Yes. International studies and Sydney Fibroid Clinic’s own studies lead by Dr Eisen Liang have demonstrated UFE (also known as UAE) is highly effective for adenomyosis as well.
More information on Sydney Fibroid Clinic’s adenomyosis treatments can be found here.
-
Am I a candidate for UFE?
If you’re troubled by the symptoms of fibroids and looking for alternative to hysterectomy, UFE offered by Sydney Fibroid Clinic could be an ideal fibroids treatment – especially if you wish to preserve your uterus, avoid major surgery and recover quickly.
To see if are a suitable candidate for UFE, call us or book a consultation with Dr Eisen Liang our Sydney fibroid embolisation specialist.
-
What pre-procedural evaluations are required for UFE? Why do I need an MRI?
All patients are required to have a pre-procedure consultation with our interventional radiologist. This allows us to obtain a gynaecologic and general medical history, review imaging findings, go through all treatment options and answer any questions regarding UFE.
An MRI of the uterus is required. MRI with DWI is needed to rule out sarcoma ( a malignant tumour that can look like a fibroid on ultrasound).
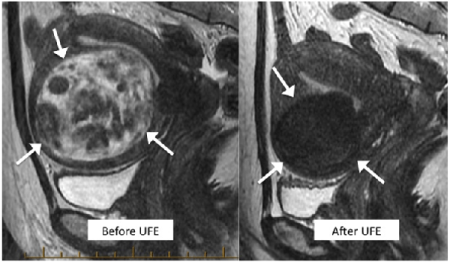
MRI also maps out fibroid locations, demonstrates richness of cells and blood supply. It helps to identify potential trouble making submucosal fibroids that might require pre-UFE Zoladex or post-UFE adjunct surgical removal.
The MRI is also used as a baseline for follow-up evaluation at six months.
The MRI needs to be done by our preferred MRI service providers, who are familiar with our stringent protocols and have fast online viewing arrangement with us.
Patients must not be pregnant. A pregnancy test is required if there is possibility of pregnancy and the procedure is done more than 10 days since the beginning of your last menstrual cycle.
-
What do I do on the day of my UFE?
On the day of your procedure, you’ll need to avoid solid food for 6 hours. Clear fluid and medications are allowed up until the time of procedure.
Nursing staff will start an intravenous line to give you fluid, sedatives and pain relief medications. We’ll also need to place a catheter in your bladder, to ensure your bladder remains empty during the procedure. As your bladder is in front of your uterus, X-ray dye collected in the bladder will obscure our view.
-
How do I recover after UFE?
After your procedure, you’ll need to lie still for 2 hours to prevent bleeding in the groin.
You may experience pain and nausea. Medications are prescribed to control these symptoms and you may ask the nurses if you require them. The pain is worse in the first 12 hours. You’ll be given a patient-controlled analgesia (PCA) pump that allows you to administer the dose you need. You are allowed to eat and drink, but you might be nauseous and you might not have any appetite.
Typically, you will no longer require the PCA the next morning and the bladder catheter can be removed to allow you to move around and to shower. The majority of our patients are able go home, though some might need to stay another night until the pain is under control and oral fluid intake is adequate.
Take home medications typically include regular Panadol and nonsteroidal anti-inflammatory drugs (NSAIDs). Additional long and short acting pain medications are also supplied. Coloxyl with Senna is also provided to prevent constipation.
In the next few days, you may experience residual pain, lethargy and low-grade fever. You should be well enough to go to the local shops on days 4 – 5. You should anticipate returning to work and normal activities about 1 week after your procedure.
Some vaginal discharge and minor bleeding is normal after UFE.
-
What follow-ups are required after UFE?
We will touvh base with you via email at 3 months post UFE to check your clinical progress. You’ll need a progress MRI at 6-month review with Dr Liang.
-
Can my GP refer directly to Interventional Radiologists for fibroids?
Yes. Interventional radiologists are clinical specialist that your GP can refer you for a seond opinion. UFEs @ Sydney Fibroid Clinic are performed by interventional radiologist Dr Eisen Liang who is specialises in fibroid embolisation.
Sydney Fibroid Clinic believes in a multidisciplinary approach to deliver the best care for women with fibroids.
You might have seen your own gynaecologist, who may or may not be familiar with UFE. Dr Liang is happy to discuss your case with your gynaecologist if needed. Otherwise, we are happy to see you to provide you with a second opinion.
If you have not seen a gynaecologist, Dr Liang is will see you first and discuss all your treatment options.
Dr Liang often consult in an adjacent room to a gyanecologist who can be invited in for a joint consultation to discuss your options. The second specialist will often bulk bill to reduce your out-of-pockt fee.
-
Are there any problems I need to watch for after UFE?
During the first week, you might experience residual pain, lethargy and low-grade fever. Minor vaginal discharge or bleeding and passage of small tissue fragments are also expected. These are normal
If the vaginal discharge is smelly, there could be bacterial colonisation and antibiotics may be required. You should see your GP or contact us for antibiotic treatment. Passage of larger fibroid fragments may be associated with pelvic cramps. Panadol and Nurofen can be used for pain control.
Resurgence of severe pelvic pain, fever, chills, and smelly vaginal discharge may indicate cervical blockage and infection. You may require urgent medical assessment. If any of these symptoms occur, please contact us immediately, or see your GP or gynaecologist. If symptoms are serious and urgent (e.g. after clinic hours), you should visit the emergency department for assessment and ask emergency doctors to contact Dr Liang via the hospital switch (the hospital where you had UFE).
Some women are able to pass fibroid fragments themselves; others might require a transcervical removal (like a curette procedure).
The risk of needing a hysterectomy to treat an uncontrollable infection is less than 1%.